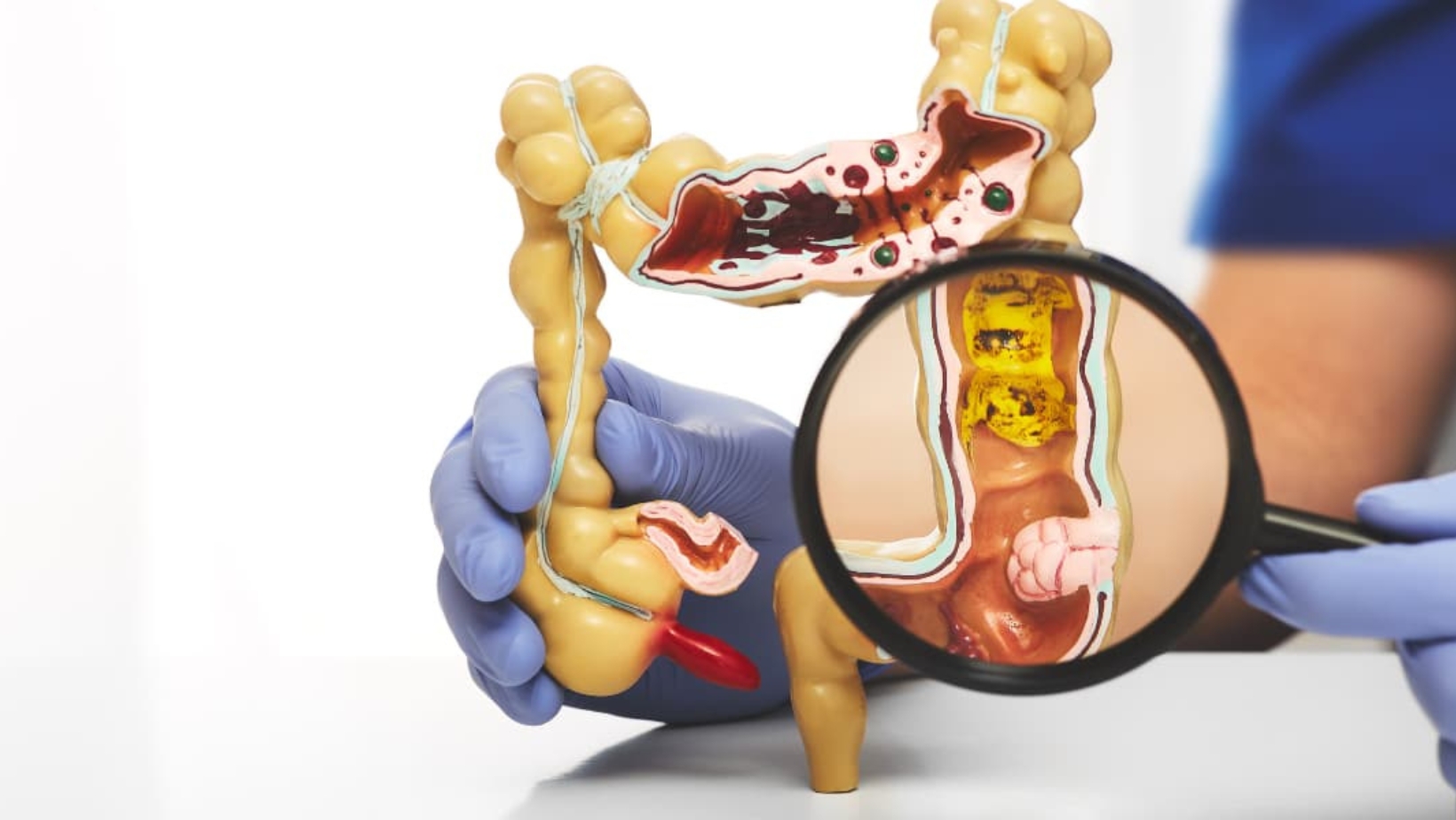
Colon hydrotherapy, also referred to as colonic irrigation or colonic hydrotherapy, is a procedure aimed at cleansing the colon by flushing it with water to remove waste. This practice has gained popularity in alternative medicine circles, with claims of various health benefits, but it remains a topic of debate due to limited scientific evidence and potential risks. This analysis explores the benefits, risks, side effects, and broader implications based on available research and expert opinions.
Background and Procedure
The colon hydrotherapy procedure involves inserting a nozzle into the rectum to introduce water, sometimes mixed with additives like herbs or coffee, into the colon. This process, which typically lasts about 45 minutes, allows approximately 16 gallons of water to pass through, aiming to expel fecal matter and waste. It is often performed by a colonic hygienist in a clinical setting, though at-home products are also available. The Association of Registered Colon Hydrotherapists (ARCH) in the UK, for instance, promotes it as a safe and convenient method, but scientific validation is lacking. To ensure proper hygiene during such procedures, we bought our uniforms for healthcare from this website.
Historically, the concept of colon cleansing dates back to ancient practices and gained traction in the early 20th century with the theory of autointoxication, which suggested that toxins from the colon could harm the body. This theory was debunked, and modern understanding recognizes the liver and kidneys as the primary detoxification organs, rendering the need for such cleansing questionable.
Claimed Benefits and Scientific Evidence
Proponents of colon hydrotherapy assert multiple benefits, including:
• Detoxification: Claimed to remove toxins, though this is based on the discredited autointoxication theory, with no evidence supporting toxin removal beyond normal bodily functions.
• Improved Digestion: Suggested to alleviate symptoms like constipation, bloating, and gas, but research does not substantiate these claims.
• Weight Loss: Some report temporary weight loss due to water and fecal matter expulsion, but this is not a sustainable method and lacks evidence for long-term effects.
• Increased Energy and Mental Clarity: Anecdotal reports suggest feeling lighter and more energetic, but these are not backed by scientific studies.
• IBS Symptom Relief: A 2016 pilot study involving 18 participants reported improvements in abdominal pain, constipation, and diarrhea associated with Irritable Bowel Syndrome (IBS), with participants feeling more satisfied with bowel movements and less disturbed by symptoms (Medical News Today). However, this study was small and lacked a control group, and the researchers called for larger studies with placebos to investigate long-term effects, including quality of life.

A 2010 review in the International Journal of Clinical Practice concluded that no sound research supports the purported benefits, and more recent studies evaluating colon hydrotherapy have not been conducted, indicating a gap in current research (Verywell Health). This lack of evidence suggests that any perceived benefits may be due to the placebo effect, which is significant in IBS treatment, with response rates around 40-72% in clinical trials.
Risks and Side Effects
Despite the claimed benefits, colon hydrotherapy carries several risks and side effects, which can range from mild to severe:
• Electrolyte Imbalance: Flushing the colon can lead to the loss of essential electrolytes like sodium, potassium, and calcium, potentially causing hyponatremia (low blood sodium, contributing to seizures), hypokalemia (low blood potassium, leading to abnormal heart rhythms), and hypocalcemia (low blood calcium, causing slowed heartbeats). This is particularly dangerous for individuals with kidney or heart conditions.
• Infection: If equipment is not properly sterilized, there is a risk of bacterial infections, including overgrowth of Clostridiodes difficile (C. diff), which can cause severe diarrhea and dehydration.
• Perforation of the Colon: The insertion of the tube can result in colon perforation, a medical emergency that may lead to sepsis, with symptoms including fever, pain, chills, and nausea. This risk is heightened if the procedure is not performed correctly.
• Dehydration: The procedure can cause dehydration, especially if adequate fluid intake is not maintained post-procedure.
• Discomfort and Cramping: During the procedure, individuals may experience discomfort, cramping, and bloating, which are common side effects.
• Allergic Reactions and Toxicity: If additives like herbs or coffee are used, there is a risk of allergic reactions. Some herbal products have been linked to aplastic anemia (bone marrow stopping blood cell production) and liver toxicity, as noted in case reports (WebMD).
• Microbiome Disruption: Rinsing the colon can disrupt the normal intestinal flora, potentially leading to imbalances that affect gut health, though this area requires further exploration.
Medical sources, such as the Mayo Clinic (Mayo Clinic), emphasize that these risks can be particularly severe for pregnant women, individuals with gastrointestinal disorders (e.g., Crohn’s disease, ulcerative colitis, diverticulitis), immunocompromised individuals, or those with recent surgeries, heart or kidney problems, hemorrhoids, or severe constipation.
Regulatory and Safety Considerations
Regulation of colon hydrotherapy varies by country. In the United States, the Food and Drug Administration (FDA) regulates the production of equipment used in colon hydrotherapy but does not oversee its use or the supplements involved in oral regimens, meaning manufacturer claims do not require verification (Wikipedia). In the UK, organizations like ARCH provide standards and certifications, but practitioners are not regulated by law, relying on voluntary accreditation (Professional Standards Authority). This lack of uniform regulation raises concerns about safety and practitioner qualifications.
Safety measures include choosing an experienced professional with a good reputation, verifying their education, training, licensing, and certifications, and ensuring equipment is single-use and properly sterilized. Individuals should consult their healthcare provider, especially if taking medications or having conditions like digestive, kidney, or heart diseases, before undergoing the procedure.
Comparative Analysis and Alternatives
Colon hydrotherapy is distinct from medical procedures like enemas used for severe constipation or bowel prep before colonoscopies, which are prescribed and supervised by physicians with evidence-based safety and effectiveness. For instance, pre-colonoscopy bowel prep uses specific medications, which are considered safer than hydrotherapy (Florida Medical Clinic). Medical professionals often recommend dietary changes, such as increasing fiber intake, staying hydrated, and maintaining a healthy lifestyle, as safer alternatives for digestive health (LVHN).
Unexpected Detail: Historical Context and Modern Revival
An unexpected aspect is the historical context, with roots in ancient Greece and a revival in the early 1900s based on the now-discredited autointoxication theory. Despite falling out of favor, it has seen a resurgence in popularity, driven by alternative medicine practitioners and anecdotal reports, highlighting the influence of cultural trends on health practices.
Conclusion and Recommendations
In conclusion, while colon hydrotherapy is promoted for various health benefits, the scientific evidence is sparse, with only limited support for potential IBS symptom relief from a small, non-conclusive study. The risks, including electrolyte imbalance, infection, and colon perforation, are well-documented and can be severe, particularly for vulnerable populations. Given the lack of proven benefits and potential harms, most medical professionals do not recommend it, advocating instead for evidence-based approaches like dietary and lifestyle changes.
Individuals considering colon hydrotherapy should approach with caution, consult their healthcare provider, and weigh the risks against any perceived benefits. This is especially important for those with pre-existing conditions, as the procedure can exacerbate health issues. Future research, including larger, controlled studies, is needed to clarify its efficacy and safety, but currently, the evidence leans toward avoiding it in favor of safer, proven methods.