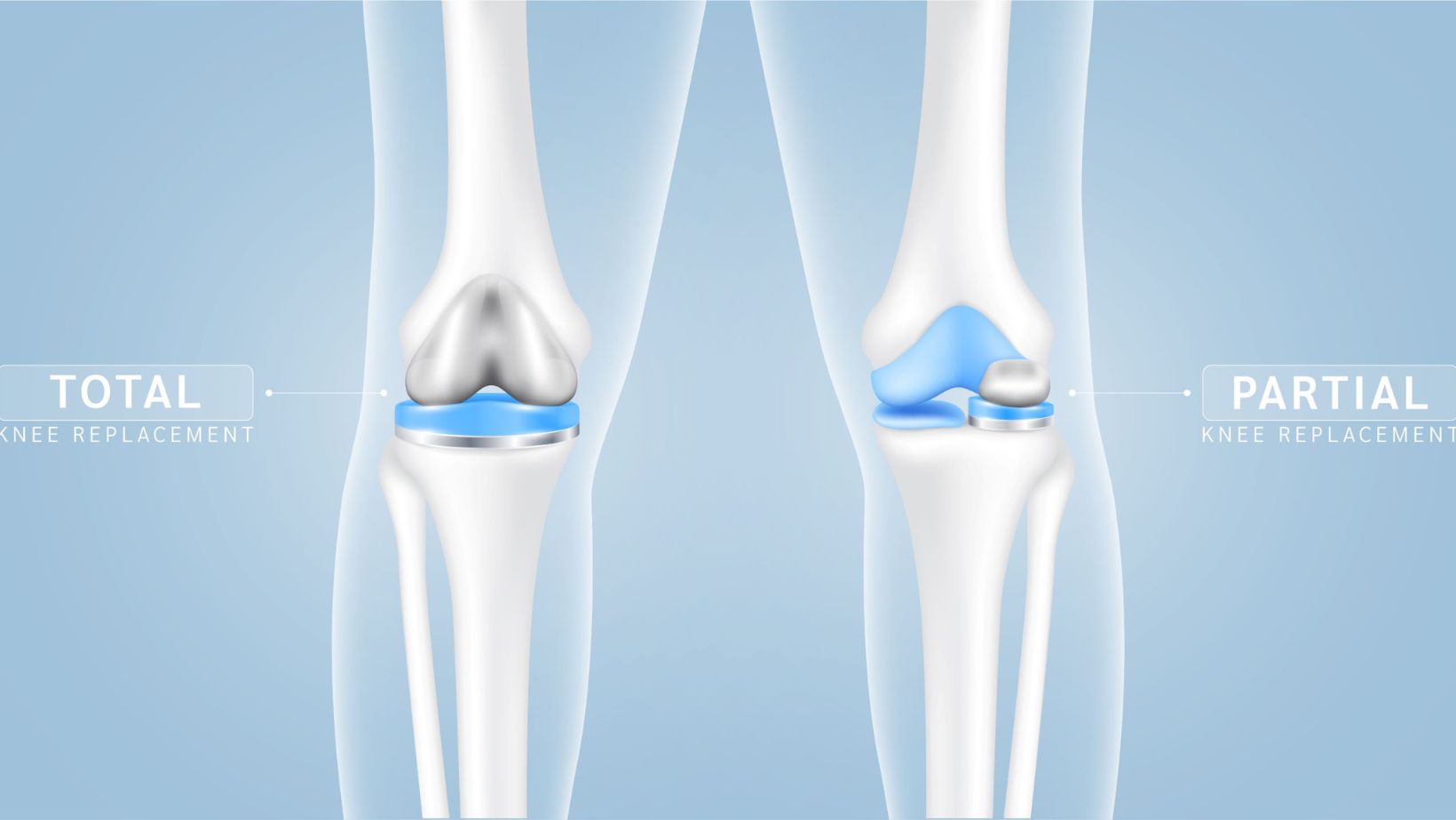
Knee replacement surgery is a transformative solution for individuals suffering from severe knee pain and mobility issues, typically resulting from arthritis or severe knee injuries. When conservative treatments like medication, physical therapy, and lifestyle adjustments fail to alleviate symptoms, surgery may become a necessary consideration. This surgical intervention can be categorized mainly into partial and total knee replacement.
By understanding the distinctions and applications of each, patients and healthcare providers can make informed decisions about the best course of treatment. But when is knee replacement necessary?
Read on to learn more.
Indications For Knee Replacement Surgery
Knee replacement surgery is typically considered for patients with persistent knee pain and functional limitations that severely impact their daily lives. This intervention becomes viable when symptoms stemming from degenerative joint conditions—such as osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis—have not improved with non-surgical approaches.
Furthermore, the decision to proceed with surgery is based on several critical factors:
- How severely the knee joint is degenerated;
- Whether the damage is localized to one part or involves multiple areas of the knee;
- Younger patients might have different considerations compared to older adults;
- Higher activity levels might necessitate a more durable solution;
- Co-existing medical conditions can influence the decision and potential outcomes of surgery.
These factors can help determine the necessity, timing, and type of knee replacement to best restore function and relieve pain.
Partial Knee Replacement Procedure
For patients whose knee damage is limited to a specific compartment, partial knee replacement surgery might be the most appropriate surgical option. This procedure involves replacing only the damaged part of the knee, preserving as much of the natural knee structure as possible. The benefits of this approach include a quicker recovery time, less pain post-surgery, and more natural knee movement compared to a total knee replacement.
However, patients and healthcare providers wanting to know more about a partial knee replacement procedure, may speak to experienced professionals or visit reputable online resources to obtain more insights.
Total Knee Replacement: When Is It Necessary?
Total knee replacement, on the other hand, is considered when the knee joint is extensively damaged. This procedure involves removing and replacing the entire knee joint with artificial components.
It’s typically recommended for patients with advanced arthritis affecting multiple compartments of the knee or those whose entire knee structure has degenerated. The primary goal of total knee replacement is to restore function, reduce pain, and enhance the overall quality of life.
Comparing Outcomes: Partial Vs. Total Knee Replacement
The choice between partial and total knee replacement is dictated by the extent and location of the joint degeneration. Partial knee replacements, which target only the affected knee section, are less invasive and involve minimal bone removal, leading to quicker recovery periods. This option is optimal for patients with localized damage.
In contrast, total knee replacements are advised for more severe cases where the degeneration spans multiple areas of the knee. Although this procedure is more comprehensive, involving the replacement of the entire knee joint, it offers greater durability and longevity, which reduces the likelihood of needing future revision surgeries. Each type serves distinct patients’ needs based on the specific conditions of their knee degeneration.
Recovery And Rehabilitation
Recovery and rehabilitation are pivotal to achieving the best outcomes after knee replacement surgery. For patients undergoing partial knee replacement, the recovery timeline is typically shorter, often enabling them to walk unassisted and resume daily activities sooner than those with total knee replacement.
However, both surgical approaches require a dedicated rehabilitation program. Such programs are designed to help patients regain knee function through tailored physical therapy sessions that focus on improving joint mobility and strengthening the muscles around the knee. The intensity and duration of rehabilitation may vary based on individual recovery rates, the type of knee replacement performed, and the patient’s pre-surgery physical condition.
Risks And Considerations
Knee replacement surgeries, like any surgical interventions, are associated with certain risks and complications. Some common issues include infections at the surgical site, the formation of blood clots, wear and tear on the implant, and, occasionally, the need for revision surgery. The likelihood of experiencing these complications depends largely on the type of knee replacement, the surgical environment, and the patient’s adherence to post-operative care protocols.
Additional factors such as the patient’s age, pre-existing health conditions, and lifestyle choices (like smoking or activity level) also play significant roles in influencing both the short-term and long-term risks associated with knee replacement surgeries. Therefore, patients must follow all medical advice and attend follow-up appointments to monitor their recovery and mitigate potential risks.
Final Thoughts
With the information mentioned above in mind, deciding when knee replacement is necessary and whether to opt for a partial or total knee replacement involves careful evaluation of the patient’s specific condition, expectations, and lifestyle. While partial knee replacement offers a quicker recovery and less disruption to the knee’s natural anatomy, total knee replacement may be necessary for comprehensive relief in cases of extensive joint damage. Ultimately, the choice should be made in consultation with an orthopedic surgeon who can provide a detailed assessment and recommend the most suitable option for each patient.